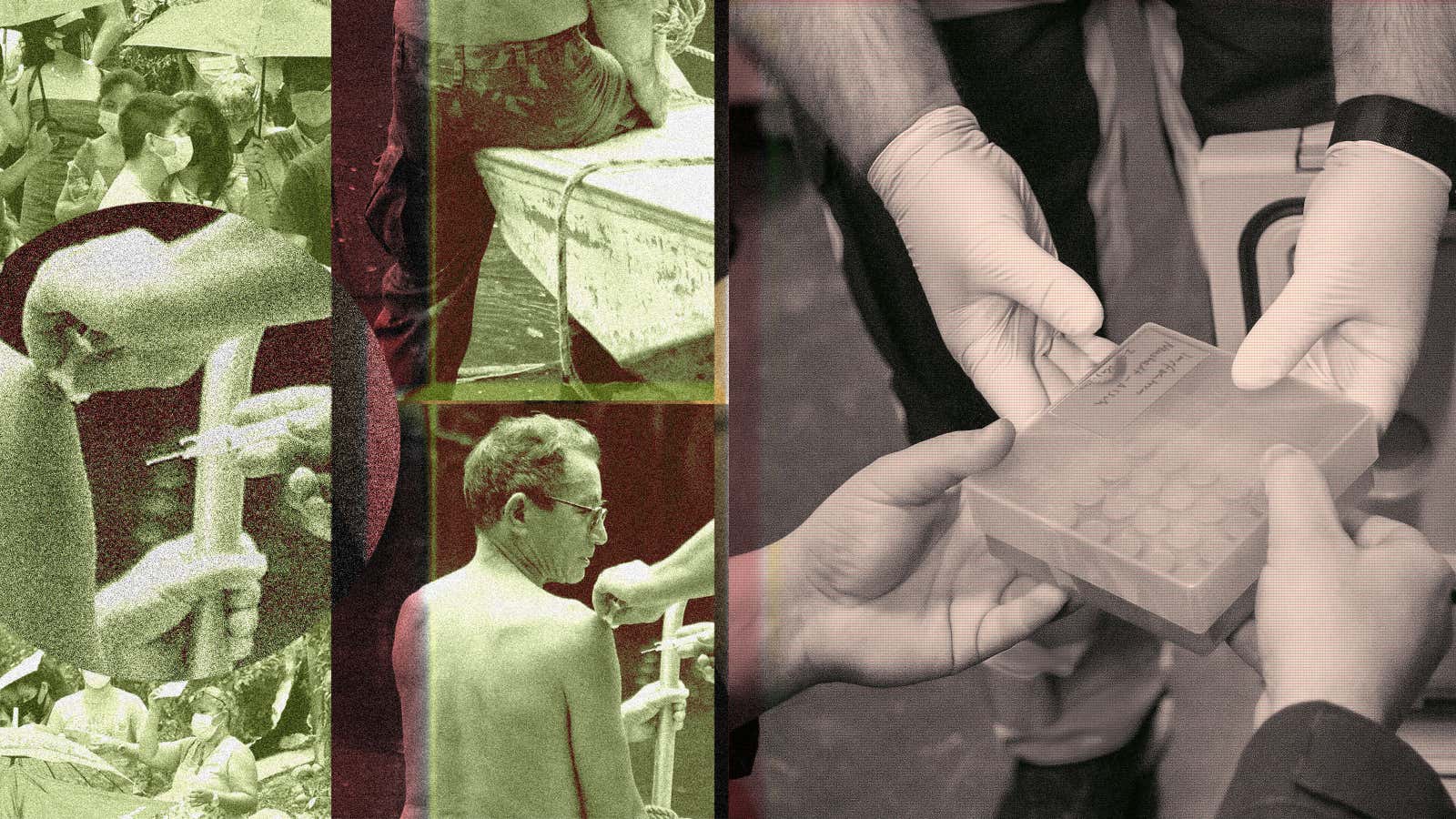
For a minute, in March of 2020, it seemed like the world was one. Cases of covid-19, yet to have a name, were popping up in every corner of the globe, uniting humanity against a common threat. Philosophizing about the virus as a great equalizer was common, as was the wishful idea we would emerge from this challenge a better version of ourselves.
The opposite turned out to be true. Since early on, the pandemic has highlighted inequality both on a micro scale—within countries, between social classes and ethnic groups—and a macro one—between rich and poor countries.
It also confirmed what many of those working in global health—particularly in and for low- and middle-income countries—expected: In an emergency, no matter the declared values and intention, people will first and foremost, and in many cases only, care about themselves and their own.
As a result, the pandemic is now proceeding at two different speeds. Most high- and upper-middle-income countries have reached and surpassed the target of having 70% of the population fully vaccinated. First booster doses have been administered, and older and vulnerable populations are being advised to get a second booster.
In the rest of the world, the situation is different. In low-income countries in particular, barely 13% of the population is vaccinated, while many countries lack even the infrastructure to accurately collect information about covid-19 cases and deaths.
Meanwhile, manufacturers of vaccines and drugs continue to refuse to share their technology and know-how, and the western countries which largely paid for their development are not putting any real pressure on them to do so.
This isn’t new, and low- and middle-income countries are reacting: They are funding their own research and development, they are working on trade agreements that bypass international organizations, and are thinking about investing in their own manufacturing capacities, shifting the power dynamic so that they are not just recipients of drugs and intellectual property, they are also makers—and potentially suppliers—of them, as well. All of these efforts are directed at tackling the current pandemic as a way to prepare themselves for when—and not if—the next one will strike, and rich countries will once again fail to rise to the occasion.
An unequal vaccine distribution system
The way the covid-19 distribution system was set up was unequal from the very beginning. Rich countries, and particularly the US and European countries, invested unprecedented sums in the development of vaccines, largely subsidizing the costs for pharmaceutical companies. In exchange for their funds, they were given priority in the allocation of available doses, and early on secured enough shots for their populations, and then some.
The rest of the world, with the exception of China and Russia, which developed their own vaccines, had to wait for the leftovers, because there simply wasn’t enough capacity to make more doses in the first few months.
Covax, a system set up by the World Health Organization (WHO) and several international organizations and philanthropies, was supposed to distribute doses sufficient to cover 20% of the population of low- and middle-income countries by the end of 2021. This was already a low target compared to the goals set for wealthy countries, which could fully vaccinate more than 70% of their population in that same period of time with their allocated doses. But even that proved too ambitious: Covax’s supply—a combination of doses manufactured by the Serum Institute of India and donations from countries with surplus doses—wasn’t reliable, or sufficient. Export regulations and initial supply crunches slowed the release of vaccines, and the doses that did get sent sometimes arrived too close to their expiration dates to be useful. By the end of 2021, the program had supplied only about 5% of global administered doses.
Countries that had heavily relied on the program, many of which are in Africa, were essentially hung out to dry. Some millions of doses were sent as charity donations through bilateral agreements—a drop in the ocean of billions more needed.
The so-called global south always knew there was going to be a shortage. So, before a vaccine became available, a group of 100 countries led by India and South Africa petitioned the World Trade Organization (WTO) to suspend patent enforcement for medications, technologies, and diagnostics connected to covid-19 for the duration of the pandemic. There were dozens of facilities available to convert to vaccine manufacturing, and many others that could have made generic versions of treatments, or diagnostics—they could have ramped up supplies relatively simply, with a little know-how help from western pharmaceutical companies, and without having to pay for licensing.
But so far there has been no agreement, and only a handful of drugmakers and their licensees and partners are producing the vaccines, in what is a de-facto monopoly over lifesaving drugs.
How wealthy countries respond to global health crises
It is not the first time that wealthy countries and big pharma have squeezed poor nations out of lifesaving drug supplies. The HIV/AIDS pandemic followed a similar pattern. Millions of lives were lost, especially in Africa and Asia, because western manufacturers didn’t allow countries like India or South Africa, which had the capacity to do so, to manufacture generic versions of the otherwise very expensive drugs they had developed.
Covid-19 confirmed that rich western nations can’t be relied upon in times of global health crises, even if they arguably have a moral obligation to compensate the rest of the world for centuries of colonialism and exploitation. Not only that, but they are stopping short of doing what they can to speed up immunization against covid-19 even as doing so has led to the emergence of new variants in countries with low vaccination rates, which then spread to all other countries. Yet even this threat to the health of their own populations hasn’t inspired a push for a less nationalistic approach to vaccine production and distribution.
“The people have the power to make changes understand [the risk] very clearly, but are just not willing to make concessions,” says Nadia Sam-Agudu, an advisor on HIV at the Institute of Human Virology-Nigeria and a professor of pediatrics in the Institute of Human Virology at the University of Maryland School of Medicine. “And not making those concessions […] relates directly to poor people dying from the diseases that are causing the pandemic—first HIV and now covid-19. And it is not acceptable in any way, shape or form.”
Preparing for the next pandemic
How can countries with limited resources tackle huge health challenges without aid from the world’s richest nations? By banding together.
A recent paper published in Molecular Therapy by Chandy John, a professor of Pediatric Infectious Disease at Indiana University’s School of Medicine and Sam-Agudu laid out the priorities that would prepare the global south—and consequently, the world—for the next pandemic. The most essential needs include stepping up local care capacity, developing pandemic preparedness operation centers that include countries of all income levels so that they can share their needs, resources, and knowledge, and promoting patent sharing and low-cost production. It also requires prioritizing vulnerable populations by identifying and eliminating racism and discrimination in any global response plan, and fighting misinformation.
The researchers also noted the importance of funding vaccine research and development in low- and middle-income countries. This is something that is already starting to happen. The South Africa mRNA hub, promoted by the WHO and funded by several organizations and countries, has a budget of about $100 million with the aim to develop and produce a locally-made mRNA vaccine, as an alternative to the ones whose licenses pharmaceutical companies haven’t shared.
“Local manufacturing initiatives like these selected by the hub can really be a game changer, because this could definitely lead to a faster and more robust scaling up of manufacturing capacity for life saving vaccines,” says Lara Dovifat, the manager of Médecins Sans Frontières campaign for access to medications.
Regional partnerships and self-sufficiency
From the WTO intellectual property waiver proposal, to setting up regional facilities such as the South Africa hub, low- and middle-income countries are collaborating with one another in an unprecedented way, independently from the input and support of rich nations. It is an important shift, because it shows a deep belief not only in the promise of self-reliance, but also that it is within reach.
“This idea that somehow we need to have high-income countries be in charge of and build the capacity for low- and middle-income countries, I think has really gone out the door in this in this pandemic,” says Matt Kavanagh, the director of Georgetown University’s Global Health Policy and Politics initiative, and a UN special advisor on HIV/AIDS.
In particular, efforts are being made to strengthen regional cooperation, readying everything from training and research to the creation of manufacturing capacity that can be used for ongoing crises as well as potential new threats, in order for it to be financially sustainable and not have to rely on emergency subsidies. Regional hubs make sense because globally low- and middle-income countries are very diverse and share disparate obstacles and needs, so it’s easier for countries in the same region, with similar challenges, to be able to work on solutions together. But it makes sense financially, too: It creates the conditions for the manufacturing of vaccines (and other therapeutics) to be sustainable as it provides a large market for the products.
“If you develop and make vaccines in one country for export to the region, the return on investment is enormous,” says Gavin Yamey, a professor of global health at Duke University. “That’s very exciting for all sorts of reasons, not just for boosting vaccine equity, but also as an investment for countries in the south.”
Who’s going to pay for it?
“Low- and middle-income countries are not penniless, right? They have resources. They do have GDPs—said GDPs might not be as big as those in high income countries, but you have that have them,” says Sam-Agudu. What is necessary is political commitment. So while the push to get wealthy country support for this and next pandemic, including through patent release, it is also essential to demand better governance in poor countries, so that health becomes a higher budget priority, and there is tangible commitment in investment.
“As much as we are impressing upon high income countries to truly approach this with solidarity and the principles of global health, we equally have to take governments of low and middle income countries to task,” says Sam-Agudu.
The idea of regional hubs and collaboration between low- and middle-income countries doesn’t rule out international cooperation. For one, the global research community has never stopped supporting the know-how development and training in the global south, and scientists working on vaccines in wealthy nations are often active participants in self-reliance efforts.
Then, there is the funding. Can countries with limited resources really build up the capacity they need, particularly when some of them still lack basic infrastructures, or the ability to provide high-technology production? Yes—and no.
Countries with limited resources don’t have the luxury to allocate much to funding systems with the sole purpose of addressing a health crisis, but that might not be necessary, or even desirable. “One of the best things to do is actually work side by side with low and middle income countries to fund disease fighting apparatuses and capacities. That’s how we get long term capacity to fight future pandemics, rather than trying to invest only in those things like laboratories that will only be used at some point in the future,” says Kavanagh.
Highly sophisticated vaccine research and production capabilities aren’t going to help in future pandemics or even ongoing health crises without strengthening basic local infrastructure to take care of non-emergency situations. Endemic health challenges could benefit enormously from investments made in research, development, and production of new medical technologies, so it’s a matter of investing in hubs that can easily be repurposed to tackle different needs—such as developing vaccines for neglected tropical diseases, or infectious diseases that largely affect low-income countries.
Naturally, the funding and technical assistance support from wealthy countries and international organizations is still important to support development of regional vaccine manufacturing hubs and an ecosystem in Africa. However, grant funding should be channeled in a way that promotes investments for future sustainability and commercial viability, rather than white elephants says Zeynep Kantur, the incoming manager for health and education at the World Bank’s International Finance Corporation (IFC).
The IFC is supporting vaccine production projects by the Institute Pasteur de Dakar in Senegal, the Rwandan government, and Biovac and Aspen Pharmacare in South Africa. The organization isn’t directly involved with the mRNA hub in South Africa, but is following it closely. “It is an R&D initiative that could change the landscape,” says Kantur.
The regional nature of the production would allow to involve various countries based on their manufacturing capacity. “It’s not that every country should try to produce everything,” says Kantur “But even countries you wouldn’t think have what it takes to be a vaccine manufacturer can be a major player in the ecosystem in terms of manufacturing something across the value chain like reagents or even plastics and the kind of materials that these vaccine manufacturing facilities will depend on.”